Next generation microsatellite instability test
Colorectal cancer, also known as bowel cancer, is the sixth most common cancer in India. National health agencies of USA, UK, France and India. recommend all bowel cancers to be tested for a specific type of “DNA spelling mistakes” called microsatellite instability or MSI for short.
Tumours containing these spelling mistakes are called MSI-high, and conversely, tumours not containing these spelling mistakes are called microsatellite stable or MSS for short. People with MSI-high cancer have a favourable prognosis and respond well to new immunotherapy treatments, compared to people with MSS cancer. The current commercially available laboratory tests that are used for checking these spelling mistakes- such as fragment length analysis and immunohistochemistry- are slow, expensive, and require an expert to interpret the result. This makes them difficult to use in a healthcare setting with small budget.
Researchers at FRIGE and the Institute of Genetic Medicine, Newcastle University, UK have developed a quick, cost-effective, and high-throughput DNA test to check for these spelling mistakes in bowel cancers. This will enable the doctors to quickly and cheaply establish if there is a problem with one or more of the “spell checker” genes in any tumour. The technical name for these spell checker genes is mismatch repair genes, or MMR for short. The results of this work have been published in the PLoS ONE and Human Mutation journal.
When a cell divides, the genetic information inside them is copied too. Sometimes, errors are made during the copying process. If an error occurs within a cancer-causing gene and is not corrected, cells can start to divide quickly and lead to cancer. The MMR genes help to prevent this. People usually have two copies of each gene. If the “spell checker” mechanism stopped working because of damage to both copies of the MMR genes in the cell, that means that the genetic problem is inside the cancer itself. However, if people inherit one faulty copy of an MMR gene, this means that every cell in their body has only one working copy of the gene. They only need one more error in the working copy for their “spell checker” mechanism to stop working properly. That person is called “predisposed” to cancer and the disease is known as Lynch syndrome.
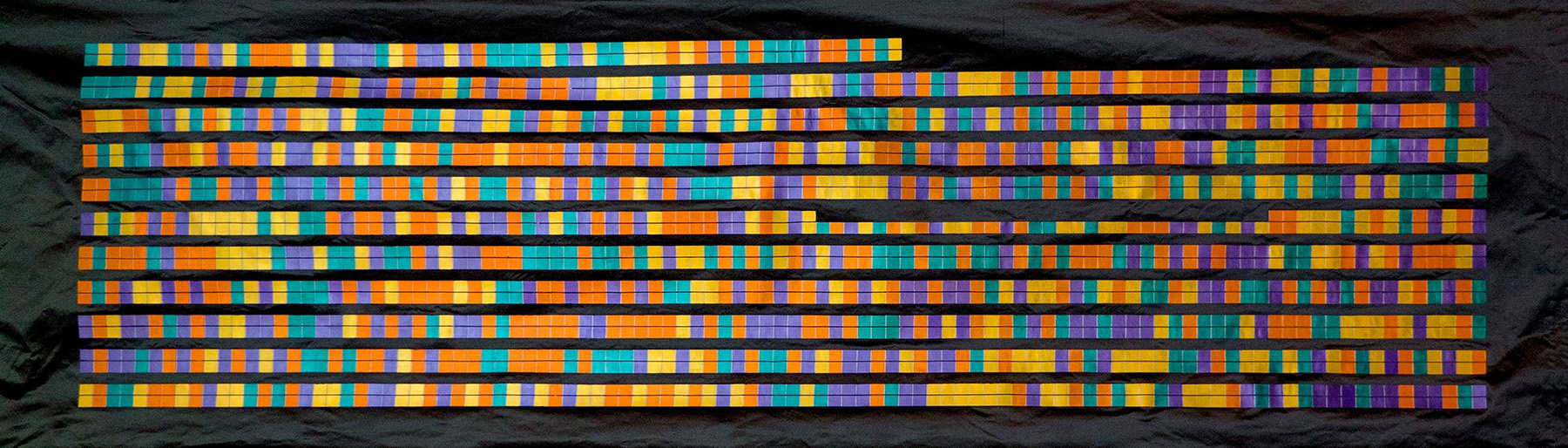
The work described here was carried out in three stages. The first stage involved identifying a novel set of short repetitive regions in the DNA, also known as microsatellites. DNA is made up of 4 letters- A, T, G and C; and all 4 letters are spread out evenly within the DNA. However, microsatellites are the regions of DNA where the same letter repeats many times. In our study, we chose microsatellites where the same letter repeated 7-12 times. Another condition for choosing a novel set of microsatellites was that they had to be next to a single nucleotide polymorphism, or SNP for short. SNPs are single letter differences in the DNA that occur between two people but don’t necessarily cause any disease. Using these two conditions meant that these regions were readable by the next generation sequencing (NGS) machines. We investigated bowel cancer DNA sequence data from the Cancer Genome Atlas database to find 120 out 218,181 microsatellites that matched our selection conditions. We then tested these 120 microsatellites in the DNA from 12 bowel cancer and 5 normal patients using NGS to identify 17 microsatellites that contained significantly more errors in the DNA of cancer patients compared to normal patients.
In the second stage, we developed a computer software that would automatically call a patient sample either MSI-high or MSS based on the sequence data from 17 microsatellites. The software uses a machine learning approach, that combines information from all 17 microsatellites. This method uses information on how many errors are there in each microsatellite and whether only one copy or both copies of DNA have these errors. Finally, this information provides a score, which suggests whether a tumour is MSI-high or MSS. The machine learning approach involved sequencing of 17 microsatellites in the DNA from 139 bowel cancer tumours that had previously been tested for MSI using commercially available tests. This gave information on how many errors occurred in each microsatellite and the number of tumours that had more errors in their microsatellites than expected.
In the final stage, we sequenced 17 microsatellites and predicted MSI status using our software for 70 bowel cancer samples. Thirty-six and thirty-four of these samples had previously been tested as MSI-high and MSS using commercially available tests. We showed that the results of our test matched 100% with those of commercially available tests.
Our test will not only help in diagnosing a cancer as MSI-high or MSS but will also help in finding those patients who have bowel cancer as a result of an inherent fault in their MMR genes. This is critical because it means that any of their relatives who also carry defective MMR genes will be at a greatly increased risk of cancer. Identifying these individuals before they get cancer means they can be offered interventions such as regular colonoscopy and aspirin to reduce cancer risk.
Our work demonstrates a novel genetic test for bowel cancer patients that is cheap and easy to run in a healthcare setting with a small budget, especially in low- to middle- income countries like India.
Currently, our research team is utilising this test in India to estimate the burden of MSI-high bowel cancers and Lynch syndrome. The research is funded by the Gujarat State Biotech Mission. Any patient with colorectal cancer is welcome to participate in the study and will get MSI and Lynch syndrome testing worth Rs. 40,000 done free-of-cost.